If you’ve ever felt a sharp twinge or a dull ache in your lower back while taking a deep breath, you know how alarming it can be. Standard medical advice—and many of our competitors—will quickly point you toward terrifying structural diagnoses: herniated discs, pinched sciatic nerves, or degenerative disease.
While these issues are real, they are often the result of a functional problem, not the root cause.
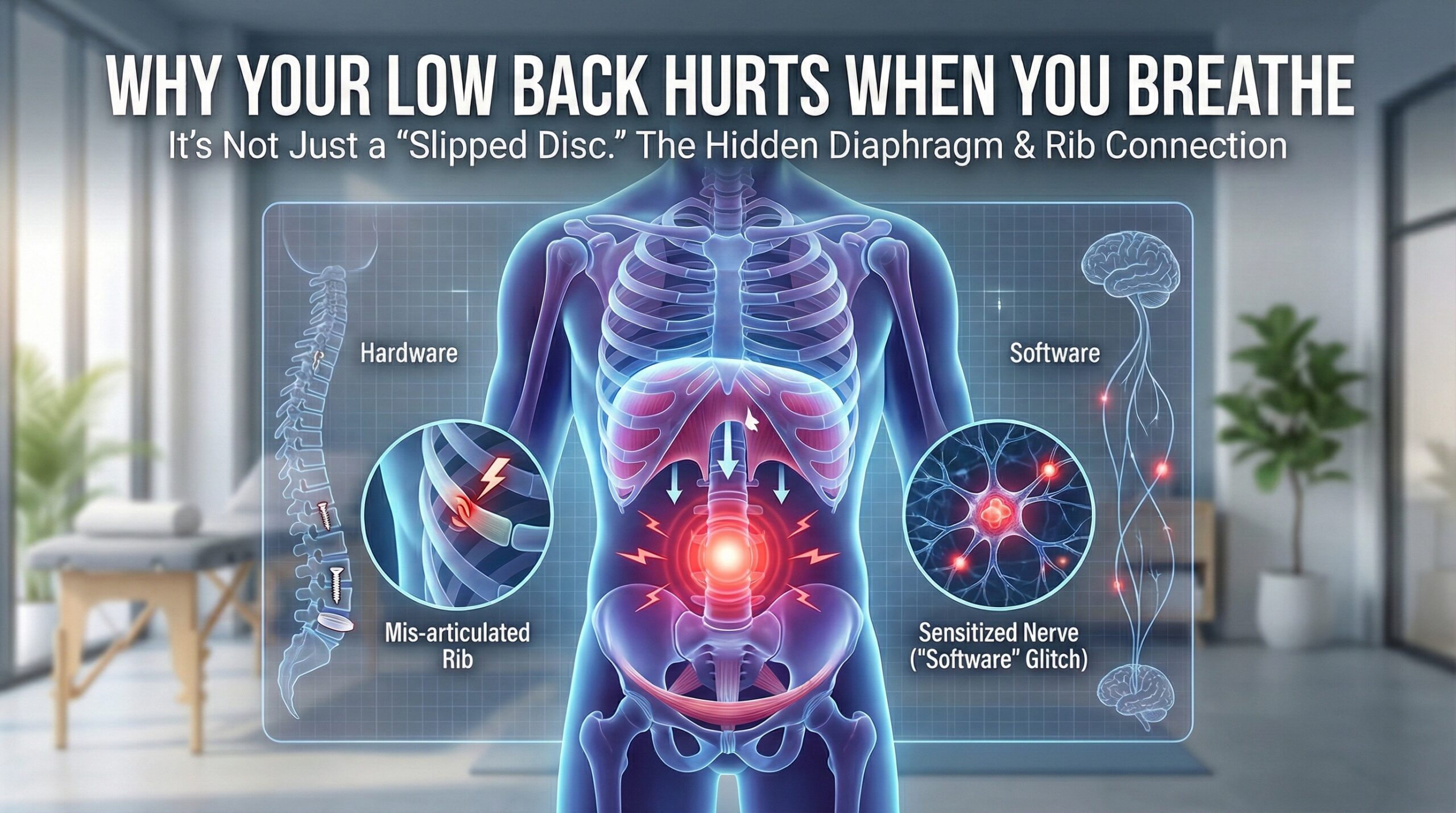
At Dr. Barber’s Clinic, we distinguish between “Hardware” problems (broken bones, ruptured discs) and “Software” problems (how your joints and nerves coordinate movement). If you only treat the pain without fixing the mechanics of how your ribs and spine move during a breath, the pain usually comes back.
Here are 5 evidence-based reasons you feel back pain when breathing, and why a precision-focused approach is the only way to fix it.
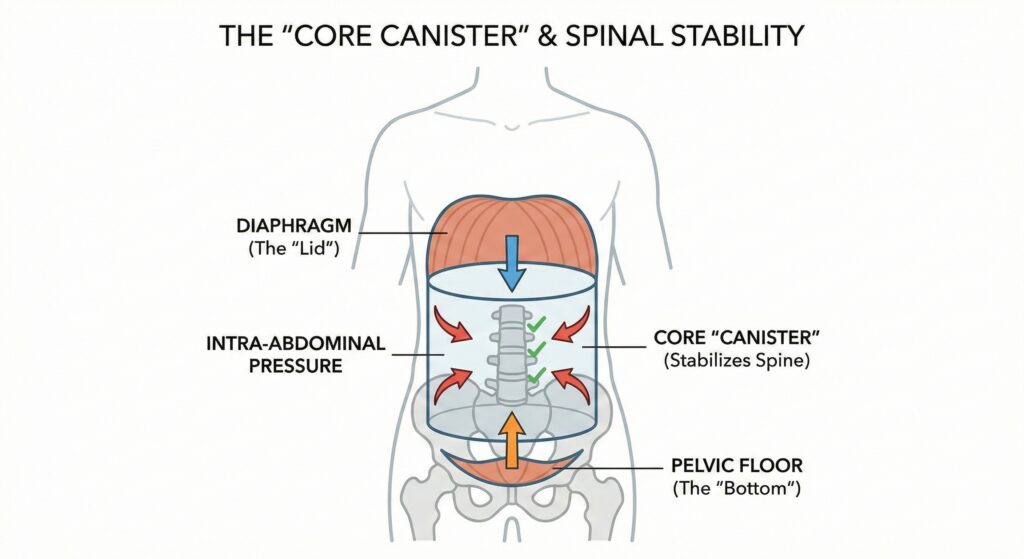
Most people think the diaphragm is just for breathing. In reality, it has two jobs: respiration and spinal stabilization.
Think of your core as a pressurized canister. The diaphragm is the lid, the pelvic floor is the bottom, and the abdominals are the walls. When you inhale, the diaphragm descends, creating intra-abdominal pressure that splints and protects your spine.
If your diaphragm is weak or fatigued, or if you are a “chest breather,” you lose that protective pressure. Your lower back muscles (like the QL and paraspinals) have to overwork to compensate, leading to pain with every breath.
The Science: A landmark study in the Australian Journal of Physiotherapy found that disorders of breathing and continence were more strongly associated with back pain than obesity or physical activity levels.¹
This is the most overlooked cause of sharp, breath-related back pain. Your ribs don’t just float in your chest; they attach to your spine via small hinges called costotransverse joints.
These joints must rotate and glide every time you inhale. If a rib joint becomes stiff or “subluxated” (slightly misaligned or stuck), it hits a mechanical block during a deep breath. This causes a sudden, sharp, or stabbing pain that can wrap around your flank. Patients often mistake this for a kidney issue or a lung problem because the pain is so visceral and intense.
The Science: Research has shown that these small joints can refer deep, dull, or sharp pain that mimics internal organ issues. A study on costotransverse joint pain patterns confirmed that dysfunction here creates significant referred pain in the back and chest wall, often requiring manual intervention to resolve.²
For a full breath, your rib cage must expand three-dimensionally. In our modern, desk-bound lives, the thoracic spine (upper back) often becomes stiff and kyphotic (rounded).
When your ribs can’t expand, your body forces movement elsewhere—usually to the path of least resistance: your hyper-mobile lower back. You aren’t feeling pain because your lower back is “bad”; you’re feeling it because your lower back is doing the job your stiff upper back refuses to do.
The Science: Research demonstrates that mobilizing the thoracic spine significantly improves diaphragmatic excursion (movement).³ If we don’t unlock the upper back, the lower back never gets a break.
If the diaphragm is the lid of the canister, the pelvic floor is the bottom. When you take a deep breath, pressure pushes down. If your pelvic floor is hypertonic (too tight) or weak, it cannot manage this pressure.
This unmanaged force is reflected back up into the lumbar spine and sacrum. This is why many patients with chronic back pain also experience subtle issues with urinary urgency or hip pain—they are all part of the same pressure dysfunction.
The Science: Effective low back rehabilitation must integrate the diaphragm and core stabilization. Treating the back muscles in isolation often fails because it ignores this hydraulic pressure system.⁴
Sometimes, the tissue has healed, but the pain remains. This is called Central Sensitization.
If you have been in pain for a long time, your nervous system becomes efficient at producing pain. The nerves in your rib cage and lower back become hypersensitive, interpreting the normal mechanical expansion of breathing as a “threat.” This requires neuro-functional inputs—like dry needling—to reset the alarm system.
The Science: A 2023 systematic review confirmed that dry needling is effective for reducing pain intensity in chronic low back pain, particularly when combined with functional therapies.⁵
The competitor down the street might offer you a generic heat pack and some stretches. Dr Jordan Barber treats the system, not just the symptom.
We specialize in the “unsolvable” cases—the patients who have tried everything else.
Stop letting pain dictate how you breathe.
Book Your Free Discovery Call with Dr. Barber