If you have been diagnosed with Complex Regional Pain Syndrome (CRPS), you are likely navigating a confusing and frustrating medical landscape. You may have been told that your nervous system is “misfiring,” or that your pain is disproportionate to your original injury.
Standard medical advice often focuses on managing this pain with medications—corticosteroids, nerve blockers, or gabapentin—and waiting for the “storm” to pass. But for many patients, management is not enough.
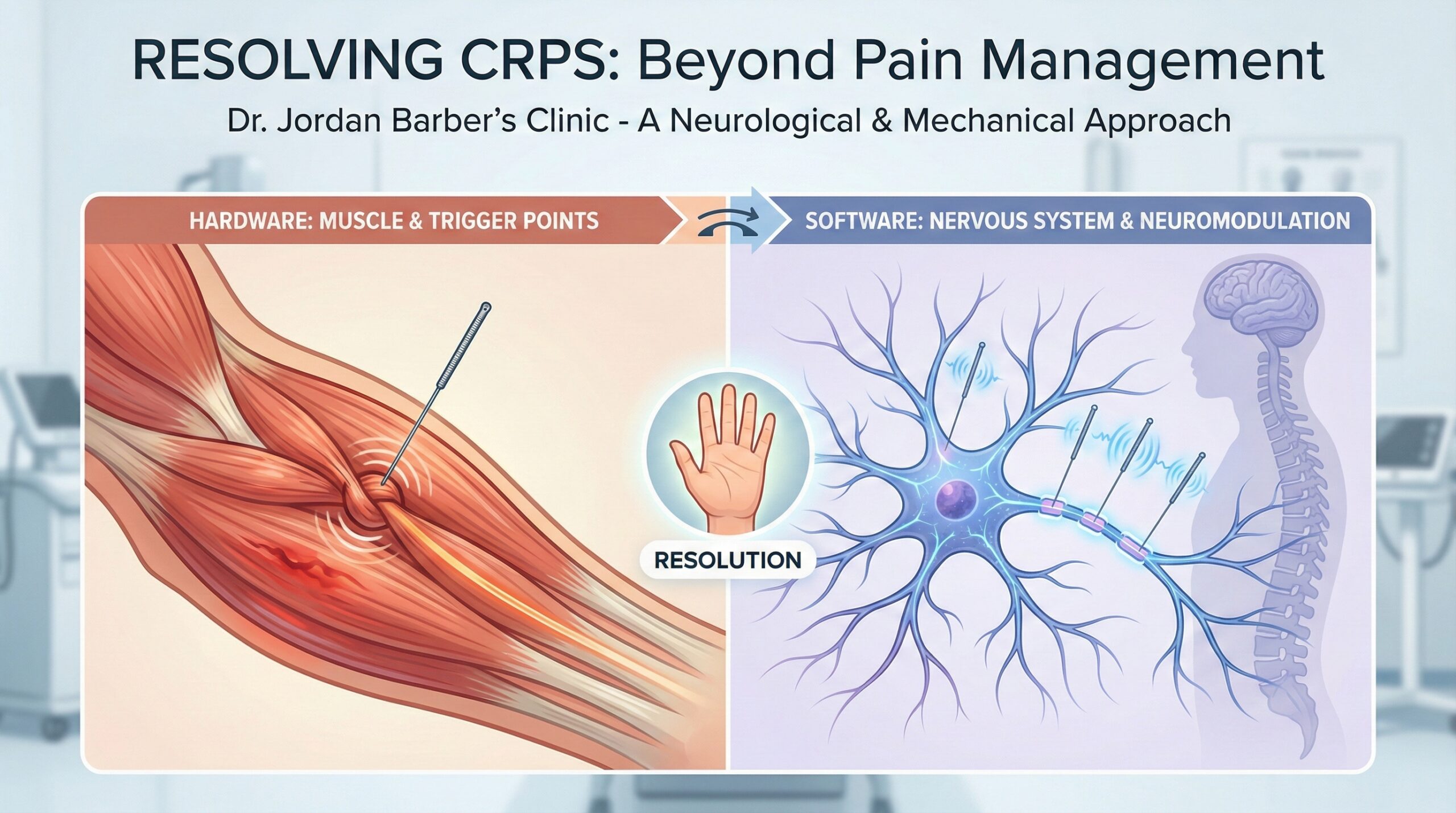
At Dr. Jordan Barber’s Clinic, we believe that to treat CRPS effectively, you must understand the mechanism driving it. It is not just “pain”; it is a malfunction of both your local tissue (the Hardware) and your central nervous system (the Software).
The conventional standard of care for CRPS focuses heavily on pharmaceutical intervention. While these treatments aim to dampen symptoms, they often fail to address the root physiological drivers of the condition.
According to a comprehensive review in Pain and Therapy, while corticosteroids and NSAIDs may offer relief in the acute (early) inflammatory phase, they show limited efficacy in resolving chronic CRPS symptoms once the condition has entrenched itself in the central nervous system [1].
Furthermore, standard physical therapy can sometimes backfire if it is too aggressive. Forcing movement through a hypersensitive limb without first down-regulating the nervous system can increase “guarding”—a protective mechanism where muscles tighten further, reducing blood flow and increasing pain.
To resolve CRPS, we have to treat two distinct problems simultaneously:
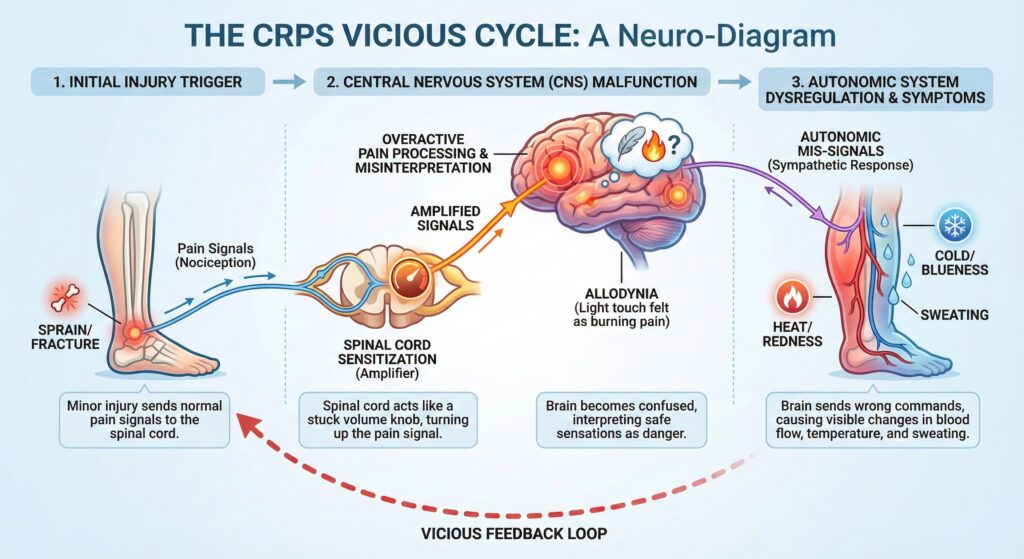
CRPS often begins with a minor injury—a fracture, sprain, or surgery. Even after the bone or ligament heals, the surrounding muscles often remain in a state of crisis. They develop Myofascial Trigger Points—tight, contracted knots of muscle fiber.
These trigger points compress blood vessels, causing local ischemia (lack of oxygen). When muscle tissue is starved of oxygen, it becomes acidic and releases inflammatory chemicals that constantly signal “DANGER” to the spinal cord. This is a physical problem that medication cannot untie.
When the spinal cord is bombarded by these danger signals for too long, it changes how it processes information. It becomes “sensitized.” This is why a light touch from a bedsheet might feel like a blowtorch (allodynia). Your nervous system has lowered its threshold for firing, interpreting safe signals as dangerous ones.
At Dr. Barber’s Clinic, we use a targeted, dual-approach to break this cycle.
Dry Needling is the most precise tool available to treat the peripheral “hardware” issues of CRPS. Unlike massage, which presses on sensitive tissue, dry needling involves inserting a thin, sterile filament needle directly into the dysfunctional trigger point.
This mechanical stimulation creates a “local twitch response,” which forces the contracted muscle to release. A study published in the International Journal of Sports Physical Therapy confirms that dry needling effectively disrupts dysfunctional motor endplates and improves blood flow (re-oxygenation) to the hypoxic tissue [2]. By physically releasing the muscle, we stop the constant stream of danger signals being sent to the brain.
Once the muscle tension is addressed, we must calm the nervous system. We utilize Neurological-Based Electro-Acupuncture, a form of neuromodulation.
By applying specific electrical frequencies to needles inserted near nerve trunks, we can communicate directly with the spinal cord. This process triggers the release of endogenous opioids (the body’s natural painkillers) and down-regulates the overactive sympathetic nervous system.
Research in the Journal of Pain Research has shown that electro-acupuncture can alleviate mechanical allodynia (pain from touch) by suppressing specific inflammatory signaling pathways in the spinal cord [3]. Essentially, we are hacking the “software” to turn off the false alarm, allowing your body to exit the “fight or flight” state and enter a state of healing.
The generalist approach of “wait and see” or “medicate and manage” is rarely sufficient for a condition as complex as CRPS. You need a provider who understands the intricate relationship between orthopedic mechanics and neurological function.
My approach is simple but rigorous:
You do not have to accept chronic management as your only option. If standard care has failed to resolve your CRPS, it is time to look at the problem through a different lens.
Schedule a Free Discovery Call with Dr. Jordan Barber Speak directly with Dr. Barber about your history and determine if our neuro-functional approach is the right path for your recovery.
References: