If you have visited a general practitioner or a physical therapy clinic in NYC recently, you might have seen the word “Dorsalgia” on your paperwork. It sounds specific, serious, and authoritative.
In reality, “Dorsalgia” is just the Latin word for “Back Pain.” It is a generic billing code (M54.9), not an explanation. It tells you where you hurt, but it tells you absolutely nothing about why.
To “diagnose” this vague condition, many modern clinics will immediately reach for a Diagnostic Ultrasound. They will scan your lower back, point to a grey fuzzy spot on a screen, and tell you that is the problem. It looks impressive—high-tech screens, fancy probes, and a “guided” procedure.
But here is the uncomfortable truth: In the vast majority of low back pain cases, that ultrasound is unnecessary. It often serves to increase the billable cost of your visit (especially in out-of-network settings) under the illusion of adding value.
At Dr. Barber’s clinic, we prefer transparency over theater. We don’t just “look” at your pain; we feel it, find it, and fix it. Here is why we prioritize Tactile Precision over unnecessary imaging.
We aren’t anti-technology. In fact, Dr. Barber has published peer-reviewed research on the use of ultrasound-guided dry needling. We know exactly how to use it, and we know exactly what its limits are.
Because we understand the science, we also understand the necessity. Research consistently shows that for most standard musculoskeletal conditions, ultrasound-guided needling does not yield significantly better outcomes than palpation-guided needling performed by a skilled clinician.¹
If the outcome is the same, why should you pay for the expensive “add-on”? We would use technology when safety demands it (like deep needling near the lungs), but for the lower back, your wallet shouldn’t suffer for a fancy visual.
An ultrasound is great at seeing fluid or tears, but it is terrible at measuring stiffness or mobility.
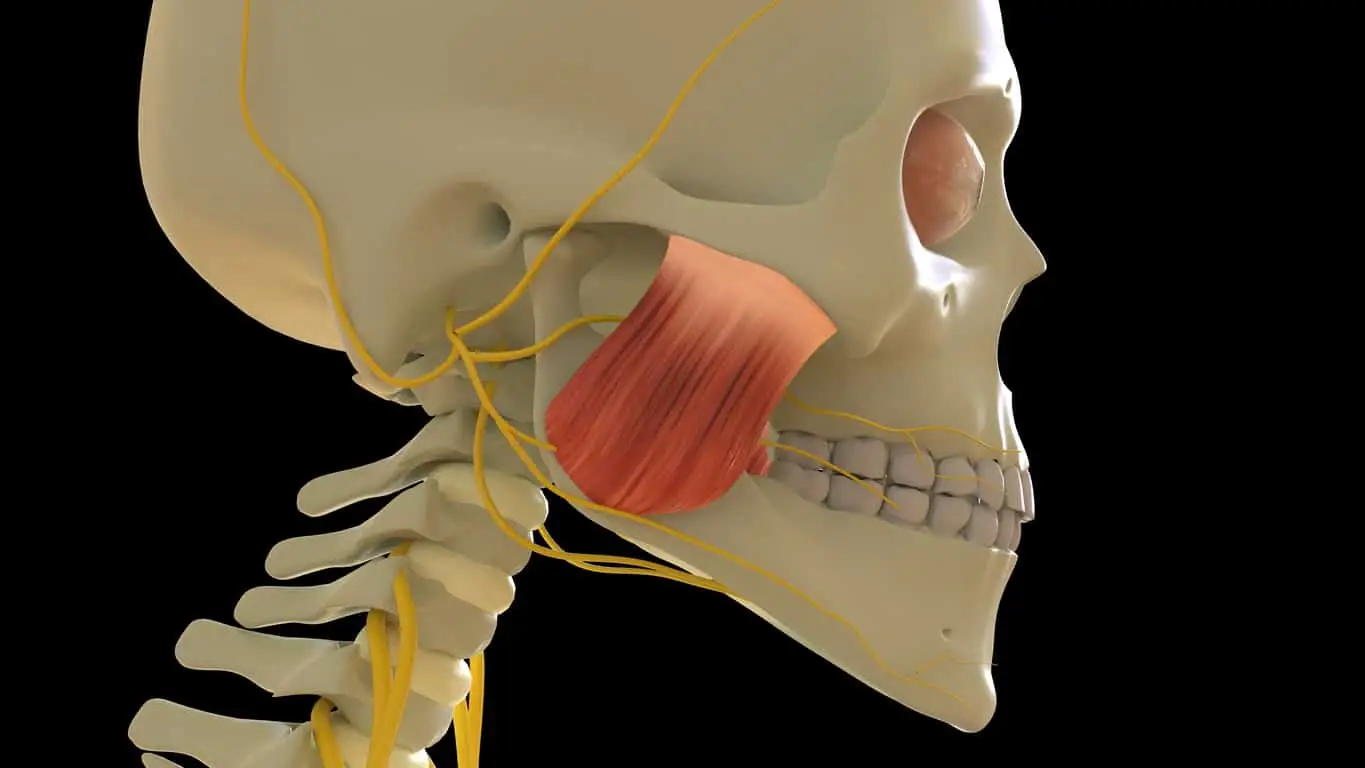
A trigger point is a 3-dimensional knot deep within the muscle belly (like the multifidus or quadratus lumborum). To truly release it, a clinician needs to feel the resistance of the tissue (tactile feedback).
When a provider relies entirely on a screen, they lose that tactile connection. They might hit the “target” visually, but miss the subtle twitch response that signals a successful release. At Dr. Barber’s clinic, we use advanced palpation-based Dry Needling. We feel exactly where the muscle is “stuck” and release it mechanically.
Chronic back pain is rarely just a “hardware” issue (a torn muscle). It is usually a “software” issue (a sensitized nervous system).
This is called Central Sensitization. Your nervous system keeps sending pain signals long after the tissue has healed. You can scan that back all day, and the ultrasound will look “normal,” but you will still be in agony.
We use Electro-Acupuncture (Neuromodulation) to target this invisible problem. By applying specific electrical frequencies to the spinal nerve roots, we hack the system, releasing natural painkillers (endogenous opioids) and turning down the volume on your pain. You cannot see a sensitized nerve on a screen, but you can certainly treat it.
Many clinics use “image guidance” to justify higher reimbursement rates from insurance companies. It creates a perception of “advanced care.”
We believe advanced care is defined by results, not props.
We treat “Dorsalgia” by ignoring the label and treating the human.
At our Upper West Side clinic, we specialize in the “unsolvable” cases—the patients who have had the MRI, the ultrasound, and the injections, but are still in pain. We don’t need a monitor to tell us you’re hurting. We need your feedback and our hands-on expertise to make it stop.
Stop settling for expensive pictures of your pain. Get a solution.
Book Your Discovery Call or an Appointment
Honest, Evidence-Based Care in NYC.